When I first started working at UVA in 2006, I had never really thought much about organ donation. But over the years, I’ve met many organ donors and recipients and helped tell their stories in one way or another. They inspired me to check the organ donor box for my driver’s license and tell my family about my decision.
This year, as we reflect on 50 years of UVA’s transplant program, I wanted to revisit some of those stories. Had those patients run into issues with rejection? What was their quality of life like? Were the family members who so selflessly donated organs also doing OK?

I caught up with three former organ donation patients: Leah Yetzer, who got a liver transplant after childbirth; Shana Roche, who gave a portion of her liver to her father; and Tina Tinsley, who got a lung transplant to treat complications of cystic fibrosis.
Leah: HELLP Syndrome & an Auxiliary Liver Transplant
In May 2009, Blacksburg resident Leah Yetzer was 36 weeks pregnant with twin boys. Her pregnancy had gone well, but that week she started having abdominal pain, headaches, swelling in her feet, and fatigue. When Leah’s OB-GYN tried to induce labor a couple of days later, her contractions affected the twins’ heart rates, and she ended up needing an emergency Cesarean section.
Her twin boys were born healthy and beautiful, but Leah’s heart rate dropped and her skin turned yellow. A medevac helicopter flew her to UVA, where doctors discovered two major problems:
- Leah had HELLP syndrome, a rare pregnancy blood-clotting disorder where red blood cells break down, and the patient has elevated liver enzymes and a low platelet count
- During her c-section, one of her arteries had unknowingly been cut, causing major undetected internal bleeding that damaged her organs, especially her liver
Ultimately, Leah needed a liver transplant, but it wasn’t a conventional one. Instead, surgeons performed an auxiliary transplant, where Leah kept her damaged liver but also received a new one. The idea is that while the body relies completely on the new organ at first, the old liver slowly heals and ultimately can also function again.
Researching Organ Donation?
Learn more about transplants at UVA
Leah was at UVA for 40 days and needed help from a home health nurse afterward while her husband and other family members took care of her twins.
But nearly eight years later, all of this is just a memory. Leah and her family now live in Ferrum, Va., south of Roanoke. She’s had two more kids, who are now 3 and 16 months old. Both pregnancies were healthy with no liver problems or other complications.
Leah’s previously damaged liver has healed and is fully functioning. She stopped taking transplant-related medications in 2012 and no longer needs checkups at UVA.
She’s also become a yoga instructor and attributes her recovery partly to her pre-transplant athletic lifestyle and healthy diet. “They told me at the hospital that because I had taken such good care of myself, it allowed me to recover.”
Read Leah’s original liver transplant story.
Shana & Michael: A Living Liver Donation & a “Miracle”

In fall 2010, a doctor diagnosed Roanoke resident Michael Cox with cryptogenic liver failure and said without a transplant, he would probably live less than five years. He got on the waiting list, but things weren’t looking good.
His daughter, Shana Roche, was a match for a living liver donation, where surgeons take just part of the donor’s liver and give it to the person in need. Shana and her husband had been unsuccessfully trying to get pregnant, but that would mean she couldn’t donate. So she immediately went on birth control.
The surgery was successful, and six months later, Shana and her husband were given the green light to move forward with attempting to get pregnant. This time, they were successful on the first try.
“We just think it was a miracle,” Shana says. “Everything happened the way it should.”
Although Michael has some unrelated health issues, his new liver functions well, and he and his wife spend one night a month with their 3-year-old granddaughter, Mara. “She’s the light of their lives and our lives,” Shana says. “She was what we all needed to move forward.”
Shana had a two-year transplant follow-up at UVA and says everything looked good. She doesn’t think she’ll need another transplant-related appointment. Her only physical reminder is a scar, which she considers a beauty mark.
“I love the reminder that it gives me every day.”
Watch Shana and Michael’s living liver donation story.
Tina: Running 5Ks with New Lungs
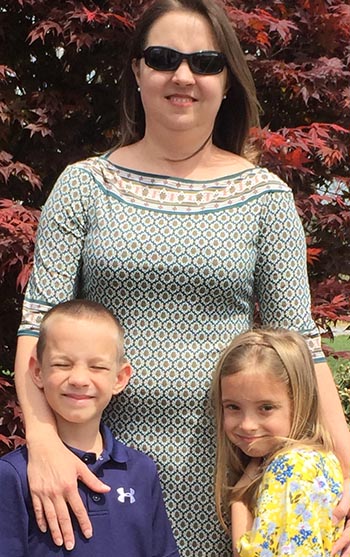
Tina Tinsley inherited cystic fibrosis (CF), a condition where the body produces excess mucus. Her condition didn’t get bad until she had twins, a boy and a girl, in 2009. By 2013, she was on oxygen and in and out of the hospital. She’d run in high school, but now, in her mid-30s, she was too exhausted and sick to even bathe her children.
In October 2013, Tina developed a lung infection, and she deteriorated to the point that she had to go on life support. Max Weder, MD, told her that without a lung transplant, she would die. This wasn’t unfamiliar territory for Tina or her family: Her brother also had CF and had been preparing for a transplant when he died at age 39. Tina’s circumstances were similar, and she feared she would die the same way he did.
But instead, after 37 days, she left the hospital with two new lungs. A couple of months later, she developed respiratory syncytial virus (RSV), a common condition that can be serious for people with lung problems, but she recovered fully.
The transplant didn’t cure her CF. Tina has digestive issues and CF-related diabetes, but her exhaustion has significantly improved. Her husband’s job keeps him very busy, so Tina is the primary caregiver for their twins, now 7. She rattles off their activities: School, baseball, horseback riding lessons and piano lessons. “I’ve gone from not being able to bathe them, clothe them, to doing primarily all of it.”
But beyond that, Tina’s also gotten back into running. When we initially interviewed her in 2014, she wanted to do a marathon. Now she says, “I think I’m finding out that I’m more of a sprinter than a long-distance runner.” She’d still like to do a marathon, but her medications, which keep her from rejecting her new lungs, cause some fatigue and leg muscle aches.
This weekend, Tina will be running a United Network for Organ Sharing 5K, which honors organ donors and celebrates recipients.
“I really have a hard time putting into words how different my life is,” she says. “I have a life, compared to before I got the transplant.”
Read about Tina’s CF and lung transplant.

