Editor’s note: I first posted about finding out I’m at high risk for breast cancer in 2021. Here's an update on how UVA Cancer Center is helping me protect my health.
“Angle your body a little more to the left. This arm up. Now look this way over your shoulder.”
It wasn’t a photoshoot. It was my first mammogram after finding out I was at high risk for breast cancer. The imaging tech helping me knew it was my first time and was really helpful in walking me through it. My doctor, Vanessa Gregg, MD, ordered the mammogram when I saw her in the UVA Health High Risk Breast and Ovarian Cancer Clinic. I happened to get it in October 2021, which was Breast Cancer Awareness Month.
Genetics play a role in about 10-15% of breast cancers and up to 25% of ovarian cancers. “We focus on breast and ovarian cancers because they can sometimes be linked in families,” Gregg explains.
In my case, Gregg recommended I rotate a mammogram and breast MRI every 6 months. That gives us the best chance to find it early if I get breast cancer. “The earlier cancer is found, the more likely a person is to survive,” she shares.
I couldn’t help feeling some alarm when I got called back for more images after my mammogram. The radiologist who read my scans was reassuring and kind. She promised me her team would always err on the side of caution. They wanted to be absolutely sure they found any cancer, so they might call me back for more images or a biopsy if there's ever a question.
Six months later, the most challenging part of my breast MRI was holding the awkward face-down position in the machine. I was relieved to get the all clear and grateful the UVA Cancer Center team was looking out for me.
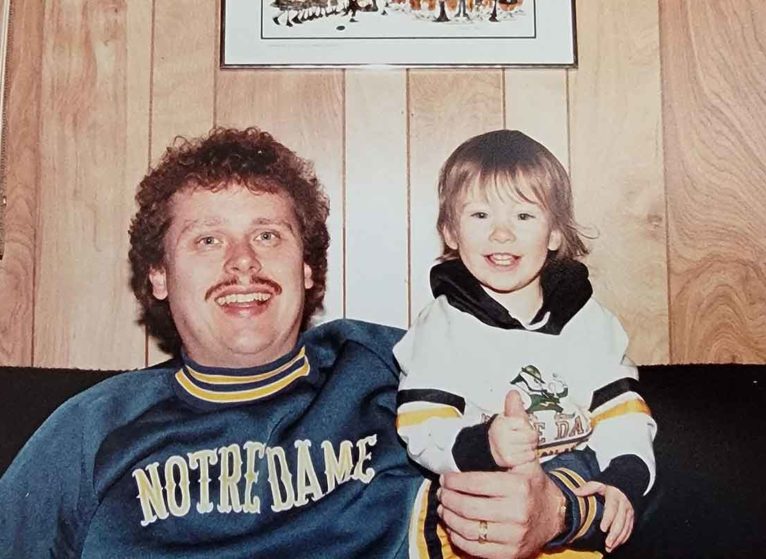
Breast Cancer in My Family
My dad, a retired general surgeon, is pretty relaxed about health issues. He keeps an “eh, it’s fine” outlook until he sees a compelling reason to be concerned. So when he said he was concerned about my breast cancer risk, I perked up.
My late grandmother had breast cancer twice, in her early 50s and 60s. She also had endometrial cancer, a cancer in the lining of the uterus, in her 50s. Her sister died from breast cancer in her 40s. My dad recently learned my half-sister also had breast cancer, around age 40. He suspected breast cancer might run in our family, putting me at higher risk. He encouraged me to look into genetic counseling and genetic testing for cancer.
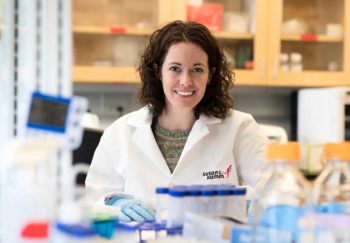
I called UVA Cancer Center and made an appointment to see Martha Thomas, MS, a genetic counselor.
Going for Genetic Counseling
At my appointment, I’m nervous and not sure what to expect, but Thomas puts me at ease. She’s thorough, so I feel confident we’re not going to miss anything.
First, we talk about my family history of cancer. She draws out my family tree, starting with both sets of grandparents. We list everyone’s siblings and children. We talk about whether each person has had any type of cancer, including what kind they had and how old they were.
In my case, I know of no one in my mom’s large extended family who has had cancer. My dad is an only child and his extended family is small. So we only know about my grandmother and half-sister.
She asks if my half-sister had genetic testing, and I can’t answer because we’re not in touch. Thomas is unphased.
"You might think your family situation is unusual, but we work with all kinds of family dynamics," she says. "We're very mindful or not wanting to create worse family communications or stress people out unnecessarily. Ultimately it’s the family’s information and how they choose to share it is up to them.”
Thomas also asks me questions about parts of my own medical history that could affect my risk.
She enters all the information into the Tyler-Cusick statistical model, a profiler that weighs all of your risk factors to tell you your personal risk.
The results say I have a 32% chance of getting breast cancer in my lifetime. The average person without my risk factors has a 10% chance. That’s shocking to hear.
Thomas tells me that my risk of developing breast cancer in the next decade is 3%, compared to 1% for someone my age with average risk. That makes me feel better.
Genetic Testing for Cancer
Next, we talk about genetic testing. Many people have heard of BRCA1 and BRCA2. But there are about 20 genes related to breast cancer risk we can test for. About 10% of patients who get these tests test positive for a genetic mutation.
Thomas explains what positive or negative results will mean. Here’s what I didn’t expect: Even if I test negative for all of these genetic mutations, we’d still consider me at high risk for breast cancer based on my family history.
The history tells us that something is causing more people in my family to get breast cancer than normal. If I test negative, it means we haven’t figured out exactly what that something is and how to test for it. We assume an unknown factor is causing more breast cancer in my family. I’m at higher risk because I might have inherited it.
What if I test positive and we figure out what was causing the family history? We would use my family history and the test results to estimate my risk.
Why Do Genetic Testing for Cancer?
The biggest reason for me to do genetic testing is that some of the genetic mutations increase your risk for other types of cancer. If I test positive, I may need to take steps to reduce my risk of getting these other cancers. One of these is ovarian cancer. Unlike breast cancer, we don’t have good screening tests to find ovarian cancer early. If I'm at higher risk, doctors might recommend I get my ovaries and fallopian tubes removed around age 40.
At the time of this appointment, I’m 37. I think about the two major surgeries I’ve already had and how much I don’t want to go through another one.
“This is a lot of information to take in,” Thomas says. “How are you feeling?”
I pause for a deep breath and admit I feel overwhelmed. But I’m really grateful for the information. I’d rather know, so I can do everything I need to do to prevent cancer.
Thomas reminds me this isn’t an emergency. I don’t have cancer yet. The profiler says I only have a 3% chance of getting it in the next decade. So we have time to get the information, think about it, and make a plan.
Thomas doesn’t push me either way on testing. I decide I want to do it, but it’s totally up to me.
“Having an appointment with me does not mean you have to go forward with testing,” she says. “Some people want to just come and hear the information. People sometimes feel like they need to be prepared for testing when all they actually need to be prepared for is to have a conversation.”
I go down to the lab. The phlebotomist takes a few vials of blood for the genetic testing, and I’m on my way.
Getting My Results
For the next three weeks, I try not to be nervous. I get an email with my results, and Thomas also calls me to tell me the genetic testing all came back negative.
Because I’m still at high risk based on the Tyler-Cusick model, Thomas refers me to the high-risk cancer and ovarian cancer program at UVA Cancer Center. My doctor there recommends I start breast cancer screenings early and do extra screenings. Now I rotate getting a mammogram and breast MRI every six months.
I feel much better knowing what my risk is and doing something about it. If I do end up getting breast cancer, I should find out within months of it developing.
“The whole point of doing genetics and high-risk screening is to allow us to be proactive about a risk as opposed to reactive about a problem,” Thomas says. “A lot of time, when we find cancers early on, they can be managed with surgery alone. You don’t have to go through something like chemo or radiation.”
I’m also grateful for the nuanced information I got from Thomas, something you can’t get from other types of healthcare providers or just reading results alone.
“We’re not only well-versed in genetics and genetic testing, but also overall risk assessment, so doing things like the Tyler-Cusick model,” Thomas says. “It’s also not specific to just one kind of cancer. We can look at the whole family history and make recommendations across the board for all types of cancer.”
Family History of Cancer?
See a genetic counselor to learn more about your personal risk for cancer.
Who Should Do Genetic Counseling?
Thomas recommends seeing a genetic counselor about your breast cancer risk if you have:
- One person in your family who was diagnosed with breast cancer under age 45
- Two people in your family who were diagnosed with breast cancer, especially if one was under age 50
- Three people in your family who were diagnosed with breast cancer
- Several people in your family with breast, ovarian, prostate, uterine, or pancreatic cancer
Does Insurance Cover Genetic Counseling and Cancer Screenings?
My private insurance covered the cost of my genetic counseling appointment and testing. This is true of most private insurances, but not Medicare. My insurance helps cover the cost of recommended breast cancer screenings.
UVA Health offers price estimates for these and other services. Some patients qualify for financial assistance based on their income.

This is SUCH a helpful overview of risk and what’s entailed in genetic counseling!!
Thanks for the clear explanation about Genetic Testing for Cancer and Insurance Coverage for Genetic Counseling and Cancer Screenings.