
The first time I heard the term “social determinants of health,” it sounded mysterious. When I finally came across the definition, however, I realized the term refers to a no-brainer.
Consider the place you grew up. Did you live in a neighborhood dense with convenience stores or farmers markets? Was it safe to play outside? Could your caregiver read English well enough to understand a prescription?
These may not seem like questions for a doctor’s office. But writing for the Ask an Expert column in the Daily Progress, Amy Salerno, MD, an internal medicine provider at UVA, says, “We know optimal health isn’t achieved during the 15-minute visit at the doctor’s office or the few days spent in the hospital; it happens outside of the clinic and hospital walls — in communities, in homes and neighborhoods.”
She’s talking about the social determinants of health, or SDOH. And she’s right. In fact, researchers have found “80% of factors that impact a person’s health are due to socioeconomic, environmental or behavioral factors.”
Defining the Social Determinants of Health
The World Health Organization defines the social determinants of health as “the conditions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels. The social determinants of health are mostly responsible for health inequities – the unfair and avoidable differences in health status seen within and between countries.”
In other words, your health directly results from your class, your environment and your culture. Belonging to a marginalized minority group plays a role. Organic produce, gym memberships, health insurance: Staying well costs money and resources.
Personal Social Health
I can definitely see how this worked in my own life. My family was poor. After my parents got divorced, my mom had to work three jobs to support us. Dinner took a backseat. We survived on fast-food drive-through windows.
By the time I got to college, I severely lacked cooking skills. Scraping by on a scholarship, I subsisted on canned goods and coffee. My dad was a smoker. I smoked. My risks for chronic disease were high. My father died of a heart attack at 52, and I was headed in the same direction.
But grad school and a job improved my socioeconomic status. That gave me time, money, health insurance and a new set of role models and values that affected my nutrition and lifestyle choices. Influenced by friends and media, I took up yoga, went vegetarian and started meditating.
No matter who you are, external factors can shape and limit your options for maintaining wellness.
Salerno summarizes this, saying, “We all are more likely to be healthier and to thrive if we live in a safe environment without fear of violence.” People also need education, a well-paying job, healthy food and affordable housing. They can thrive when not facing discrimination.
Central Virginia Health Challenges
Locally, 12,024 families in Central Virginia (PDF) do not make enough money to afford either the essentials of food, shelter, clothing and utilities or the added costs associated with working, like childcare and transportation.
The three most critical issues for our population:
- Access to healthy food
- Inactive lifestyles
- Mental health issues and substance abuse
But of course, healthcare providers by themselves can only do so much. Looking at the SDOH, we can see that our neighbors’ health depends on so much more than a single nurse, clinic or hospital. The social determinants must be addressed by the society as a whole.
Community-Wide Health Issues
Poverty, food insecurity, homelessness and illiteracy can hurt a person’s ability to:
- Fill prescriptions
- Take medication
- Dress a wound
- Manage diabetes
- See a therapist
- Buy food
And because many of these factors are environmental, we’re not just talking about individuals. As studied by Healthy People 2020, these “social determinants” affect whole communities.
Communities struggling with poverty, unstable housing, low income, unsafe neighborhoods or substandard education face increased rates of:
- Increased risk for diabetes
- Lower life expectancy
- Mental disorders
- Obesity
- Addiction/substance abuse
- Asthma
- Heart failure
- Stroke
- Cancer
Healthcare & Bias
People belonging to minority groups that experience discrimination face social barriers that play a role in health and wellness. Facing discrimination and bias on a daily basis can:
- Hurt physical and mental health
- Prevent access to care
- Weaken the quality of care received
Health Impact of Minority Stress
Constantly experiencing the strain of bias can raise anxiety and depression. One study of women and black, Hispanic, lesbian, gay, and bisexual people found that those “who reported experiences of discrimination within the past 12 months had an association between the experience of discrimination and mood, anxiety and substance use disorders.”
Physical health suffers, too. Daily stress from discrimination, rejection and internalized homophobia, for instance, weakens immune systems. This makes people vulnerable to disease.
Research has found that lesbian, gay and bisexual people who experience prejudice at a doctor’s office are more likely to have physical health problems.
Bias Within the Culture
Discrimination or a lack of equality in social and legal systems directly and indirectly result in health disparities. Two examples of communities affected in this way: LGBTQ people and people with disabilities.
We can see, for instance, oppression and discrimination interfering with the health of LGBTQ people in:
- Legal discrimination in access to health insurance, employment, housing, marriage, adoption and retirement benefits
- Lack of legal protection against violence, from hate crimes to bullying in schools
- Lack of social programs for LGBT youth, adults, elders
- Shortage of healthcare providers knowledgeable about LGBTQ health
People with disabilities report lower screening rates and more difficulty accessing health services (PDF). As a result, compared to able-bodied people, people with disabilities have:
- Higher rates of poor health
- More tobacco use
- Less physical activity
- Higher rates of obesity
Local Social Determinants & Data
Read the whole 2019 Central Virginia health assessment (PDF).
Bias Within Healthcare
Bias within the healthcare system itself often compounds health problems by creating barriers to adequate healthcare.
Several recent studies have shown the inequities in healthcare experienced by people of color. The findings illustrate the real ramifications of the problem:
- Mothers of color are three times more likely to die during pregnancy than white women
- Kids of color aren’t treated at the same rate as white kids
- Minority patients seeking care in the emergency department are 22-30% less likely than white patients to get pain relief medicine
- White people have a greater chance of getting treated for myocardial infarction than people of color
This is why Rebecca Dillingham, MD, teaches medical students about bias at the UVA School of Medicine. According to her, medical providers need to “reduce or eliminate” the impact of bias in how they treat and care for patients.
What else can healthcare professionals and community members do to close our community’s health gaps? Learn about recent wellness efforts to handle health disparities in Charlottesville.
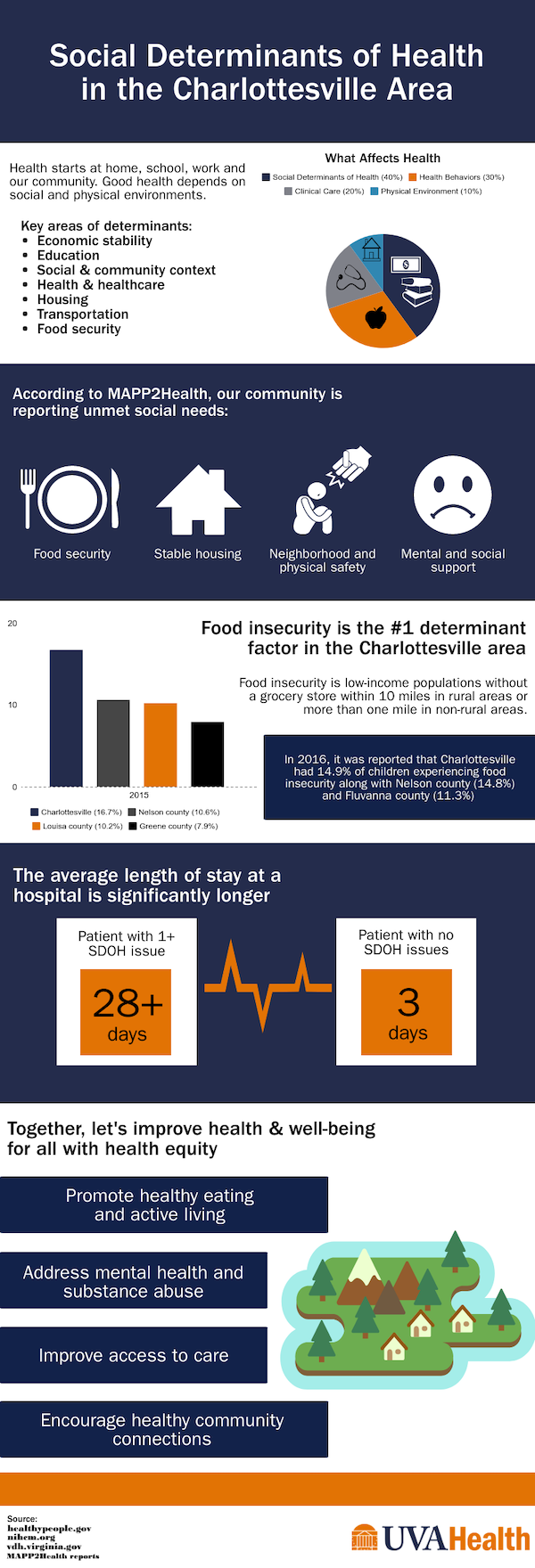
Infographic Text: Social Determinants of Health in the Charlottesville Area
Health starts at home, school, work and our community. Good health depends on social and physical environments.
- Social determinants of health 40%
- Health behaviors 30%
- Clinical care 20%
- Physical environment 10%
Key areas of determinants:
- Economic stability
- Education
- Social and community context
- Health and healthcare
- Housing
- Transportation
- Food security
According to MAPP2Health, our community is reporting unmet social needs:
- Food security
- Stable housing
- Neighborhood and physical safety
- Mental and social support
Food insecurity is the #1 determinant factor in the Charlottesville area.
Food insecurity is low-income populations without a grocery store within 10 miles in rural areas or more than one mile in non-rural areas.
In 2016, it was reported that Charlottesville had 14.9% of children experiencing food insecurity along with Nelson County (14.8%) and Fluvanna County (11.3%)
In 2015, percent of population with food insecurity:
- Charlottesville, 16.7%
- Louisa, 10.2%
- Nelson, 10.6%
- Greene, 7.9%
The average length of stay at a hospital is significantly longer:
Patient with 1+ SDOH issues = 28+ days
Vs.
Patient with no SDOH issues = 3 days
Together, let’s improve health and well-being for all with health equity:
- Promote healthy eating and active living
- Address mental health and substance abuse
- Improve access to care
- Encourage healthy community connections
Sources:
Healthypeople.gov
Nihcm.org
Vdh.virginia.gov
MAPP2Health reports

